May 2024
Dr. Girardi’s Research Grant
Congratulations are in order for Dr. Michele Girardi who was awarded a Fellowship grant from the Tobacco Related Disease Research Program. His study aims to explore how fatigue of the muscles that allow for breathing affects the ability to exercise in people with chronic obstructive pulmonary disease (COPD). Firstly, he will examine how the performance of these breathing muscles change over time during exercise. Then, he will look at how fatigue of these breathing muscles influences the decline in leg muscle performance during exercise, using a new exercise test developed at the Lundquist by some of Dr. Girardi’s mentors called the musculo-cardio-pulmonary exercise test (‘mCPET’). Additionally, he will investigate how adding or relieving the work done by the breathing muscles affects the ability to tolerate exercise. These data will significantly advance our knowledge of the basic mechanisms of exercise intolerance in COPD and our understanding of how fatigue of the muscles that support breathing affects leg muscle performance and exercise tolerance. This knowledge is essential for understanding how best to implement effective treatment strategies in COPD to alleviate symptoms and improve exercise capacity. Dr. Girardi will be supported during this Fellowship by his primary Mentor, Dr. Ferguson, and his co-mentors, Drs Rossiter, Casaburi, DeCato and Taylor. This research study will start in July 2024.

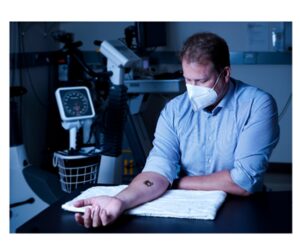
US Army Awards $2.6M to Develop Wearable Biosensors for COPD
The US Army Medical Research Acquisition Activity has granted over $2.6 million to a team led by Dr. Harry Rossiter from The Lundquist Institute and UCLA. They aim to develop a sensor that could transform COPD management by predicting exacerbations in real-time without the need for frequent blood tests. COPD is a major health issue affecting millions globally, and exacerbations, often triggered by lung infections, worsen the condition and strain healthcare resources. The team’s previous work on a wearable biosensor tracking C-reactive protein (CRP) in sweat has laid the foundation for this project. They’re now focusing on identifying additional molecules in sweat to improve the prediction of future exacerbations. If successful, this technology could significantly improve COPD care and patient outcomes.
“Our ultimate goal is to develop a wearable system to preempt AECOPD, providing an early warning system to move treatment earlier in the exacerbation process and thereby reduce patient morbidity, mortality, hospitalization, and healthcare utilization,”
– Dr. Rossiter
Wasserman Dinner and Lecture
This annual event is supported by fellows and colleagues of Dr. Karlman Wasserman to celebrate his mentorship by bringing leaders in the field of Pulmonary and Critical Care Medicine to the Harbor-UCLA campus. This year we were pleased to welcome Dr. Mark Dransfield to deliver the Wasserman Lecture. Dr. Dransfield is Professor of Medicine and Director of the Division of Pulmonary, Allergy and Critical Care at the University of Alabama, Birmingham.

New Team Members
The Respiratory Research Center is delighted to announce the expansion of our team with the addition of new members! We warmly welcome two study coordinators, Lizette Trujillo and Viviana Gonzalez, as well as two exercise physiologists, Stephanie Chen, M.S. and LeAnn Maanum, M.S. With these talented individuals joining us, we are poised to provide enhanced care to our patients and advance our Center’s mission!
RRC Member of the Month
Dr. Nicholas Jendzjowsky is an Assistant Professor at UCLA and an Investigator at the Lundquist Institute for Biomedical Innovation at Harbor-UCLA Medical Center. He is the Principal Investigator of the Neuroimmunology Lab at the Respiratory Research Center (neuroimmunelab.org). Dr. Jendzjowsky received his Ph.D. at the University of Alberta, Edmonton Canada, and studied autonomic neural control of vasomotor function. He did his postdoctoral fellowship with Dr. Richard Wilson at the University of Calgary, where he studied the role of sensory neurons in cytokine sensitivity in asthma. This forged his path in the neuroimmune landscape where he currently studies how sensory neurons regulate adaptive immunity in lung infection and asthma. In his spare time he enjoys long runs in the mountains.
Leave a reply