COPDGENE’s 15 Year Anniversary
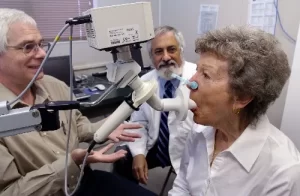
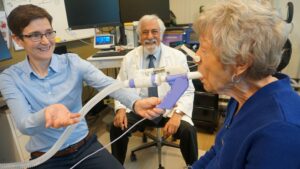
The Respiratory Research Center was pleased to welcome Mary Burns RN for her return visit as part of the COPDGene study. Ms. Burns was the first of 760 subjects studied at our site when the study began in 2008. The COPDGene study is supported by the National Institutes of Health. It was initiated to try to better understand COPD. The study’s central aim was to determine why some smokers develop COPD while others do not. The study’s success was recognized by three five-year renewals, allowing people who originally participated in 2008-2011 to return at five, ten and now fifteen years after they were originally studied. The long-term follow up of these study participants is helping us to define the factors that determine progression of COPD. Ms. Burns’ visit represents the beginning of “Phase4”: visits on the 15th anniversary of the original visit. The COPDGene study has an enviable record of success. Over 500 scientific papers have been published. A roughly equal number of “ancillary studies” have been initiated: research studies delving into the rich data base that the COPDGene study has accumulated. The investigators at the Lundquist Institute have been active in many of these publications and studies.
National Science Appreciation Day
We showed appreciation to our staff by enjoying breakfast together with Dr. Irina Petrache, Chief of the Division of Pulmonary, Critical Care and Sleep Medicine at National Jewish Health, and incoming president of the American Thoracic Society. Dr. Petrache was visiting to deliver an outstanding Samuel J. Sils Distinguished Lectureship (awarded by the Trudeau Society) at Harbor-UCLA Medicine Grand Rounds.

YMCA Community Partners Day
The Respiratory Research Center was one of the few organizations to be invited by Torrance YMCA to their event. To the adults who visited our table we talked about the cutting research going on at the Center and handed out Lundquist goodies to the kids!
RRC Member of the Month
Katelin Bebe is a volunteer research assistant at the Lundquist Institute Respiratory Research Center and a medical assistant at Beach Cities Orthopedics and Sports Medicine. She completed her Bachelor of Science with a major in Kinesiology and a minor in Pre-Health Professions at California State University, Fullerton (CSUF). At CSUF, Katelin played on the CSUF Women’s Soccer team. In addition to volunteering and working, Katelin has also been studying for the MCAT with the plan to apply to medical school this May 2024. Some of Katelin’s favorite hobbies include skiing, going to the beach, playing games/sports, hiking, and hanging out with friends, family, and her puppy, Charlie.

What is Expiratory Flow Limitation? And Why Should I Care?
So you haven’t heard of “expiratory flow limitation”? That’s not surprising. But if you know someone with asthma or COPD, then you are probably more aware of it than you think. Expiratory flow limitation, or EFL for short, is the medical term to describe a narrowing of the airways that causes increased resistance to breathing out. For patients with asthma or COPD, emptying the lungs can be difficult and slow. When breathing needs to speed up, such as during physical activity, EFL is the process that leads to the feeling being unable catch one’s breath. Breathing techniques, such as purse-lip breathing, can reduce the impact of EFL, allowing slower and deeper breathing and reducing the scary sensations breathlessness. In a recent paper, Respiratory Research Center investigator Tom DeCato, MD, and collaborators from Washington State University-Spokane and Vermont State University, trained artificial intelligence (AI) to recognize EFL based on people’s spontaneous breathing patterns. Amazingly, the AI had an accuracy of ~90% at predicting EFL; even in people with normal lung function. Dr. DeCato says “Although this research is in its early days, we hope it could lead to new diagnostic tools to help us better identify and treat those who experience EFL during physical activities.”
Leave a reply